Patient-Centered Problem Solving: Case Studies in Healthcare Delivery dives headfirst into the fascinating world of putting patients at the heart of their own care. Forget the old-school doctor-knows-best approach; we’re exploring how shared decision-making, personalized treatment plans, and truly listening to patients can revolutionize healthcare outcomes. This isn’t just theory; we’ll unpack real-life case studies showcasing the triumphs and challenges of this patient-centric model across various healthcare settings.
From managing chronic illnesses like diabetes to navigating the stressful waters of acute care and end-of-life decisions, we’ll analyze how effective communication, collaboration, and empathy transform the patient experience. We’ll also tackle the hurdles – systemic barriers, provider training gaps, and even measuring success – and explore strategies to build a more patient-centered healthcare system.
Case Study 3: End-of-Life Care: Patient-Centered Problem Solving: Case Studies In Healthcare Delivery
This case study explores the application of patient-centered problem-solving in the context of end-of-life care, focusing on the ethical, emotional, and logistical aspects involved in supporting both the patient and their family. We will examine a specific scenario to illustrate the practical application of these principles.Mrs. Eleanor Vance, a 78-year-old woman with metastatic lung cancer, was admitted to hospice care.
Her prognosis was poor, with a life expectancy of weeks. Mrs. Vance, a devout Catholic, expressed a strong desire to die peacefully at home, surrounded by her family. However, managing her pain and ensuring her comfort at home presented significant challenges. Her family, while supportive, was struggling with the emotional toll and practical demands of providing around-the-clock care.
This situation highlights the complex interplay of medical, emotional, and spiritual needs common in end-of-life care.
Ethical Considerations in End-of-Life Decision-Making
Ethical considerations in end-of-life care center on respecting patient autonomy, ensuring beneficence (acting in the patient’s best interest), and maintaining non-maleficence (avoiding harm). In Mrs. Vance’s case, the hospice team prioritized her wishes regarding her place of death. Open communication was crucial, ensuring she understood her options and the potential challenges associated with each. The team also worked to ensure her comfort and pain management, balancing the use of medication to alleviate suffering with the avoidance of unnecessary sedation that might compromise her awareness and ability to interact with her loved ones.
Discussions regarding the use of life-sustaining treatment were guided by her expressed wishes and her advanced directives, ensuring her autonomy was respected.
Strategies to Support Emotional and Spiritual Needs, Patient-Centered Problem Solving: Case Studies in Healthcare Delivery
Addressing the emotional and spiritual needs of a dying patient is paramount. For Mrs. Vance, the hospice chaplain provided regular spiritual support, offering comfort and guidance aligned with her religious beliefs. The hospice team also facilitated visits from family and friends, creating a supportive environment. They actively listened to Mrs.
Vance’s concerns and anxieties, providing emotional support and validating her feelings. The family was also offered grief counseling and support groups to help them cope with the emotional burden of caring for a dying loved one. Regular family meetings were held to address practical concerns and provide emotional support for all involved.
The Role of Family Members and Caregivers
Family members and caregivers play a vital role in end-of-life care. In Mrs. Vance’s case, her family’s active involvement was crucial to her well-being. The hospice team provided them with training on pain management techniques, medication administration, and basic caregiving skills. They also facilitated open communication between Mrs.
Vance and her family, encouraging honest conversations about her wishes and fears. Regular meetings and open communication channels ensured the family felt supported and empowered in their caregiving role. The team addressed their concerns and offered respite care to prevent caregiver burnout.
Key Elements of a Patient-Centered Approach to End-of-Life Care
Effective end-of-life care necessitates a patient-centered approach. Key elements include:
- Prioritizing patient autonomy and respecting their wishes regarding treatment and end-of-life care.
- Providing comprehensive pain and symptom management to ensure comfort.
- Addressing the patient’s emotional and spiritual needs through active listening, empathy, and appropriate referrals.
- Involving family members and caregivers in the care planning and decision-making process.
- Offering education and support to family caregivers to prevent burnout and promote effective caregiving.
- Ensuring open communication and transparency among the patient, family, and healthcare team.
- Providing access to appropriate resources, such as palliative care, hospice, and grief counseling.
Barriers and Facilitators to Patient-Centered Problem Solving
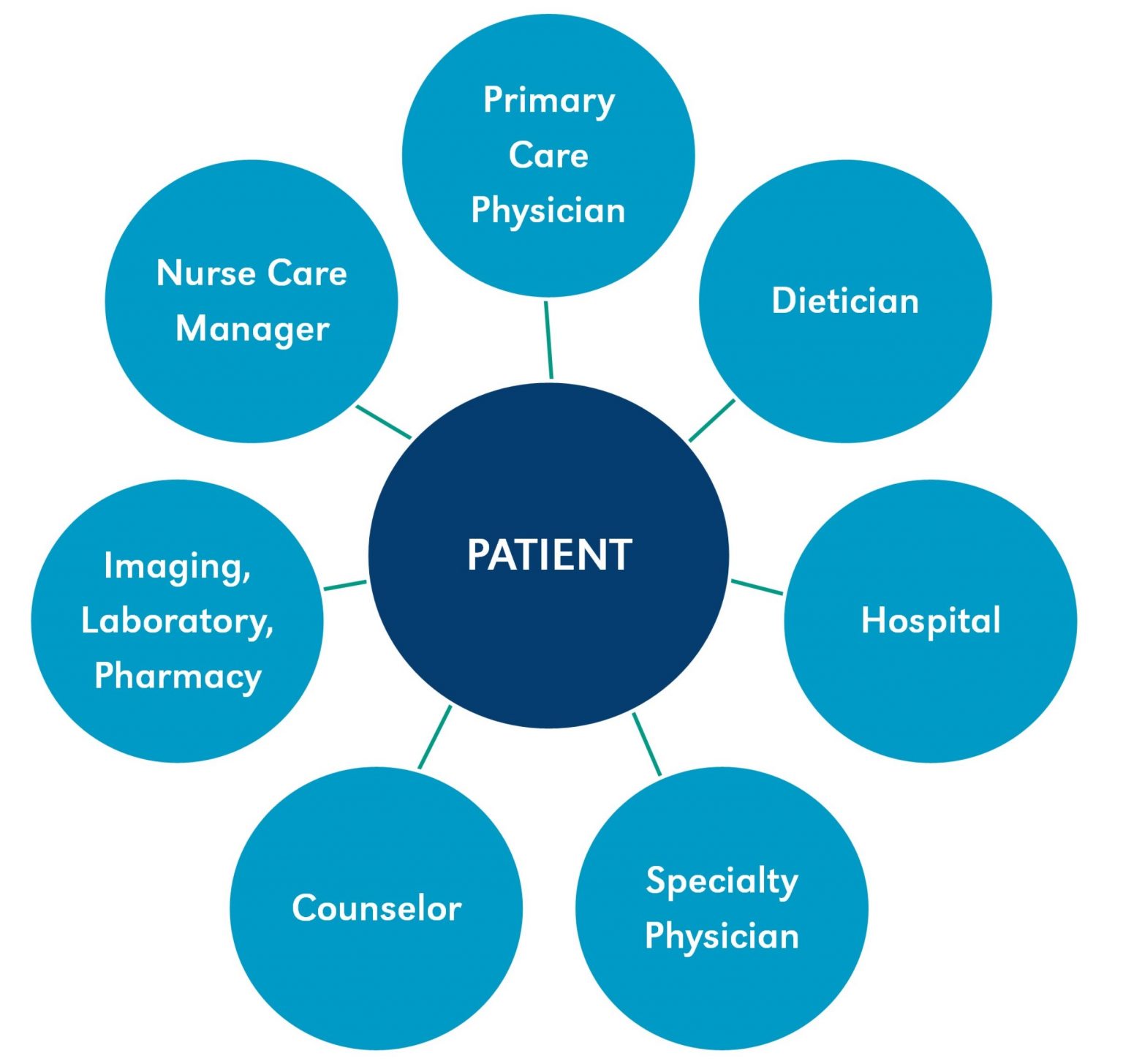
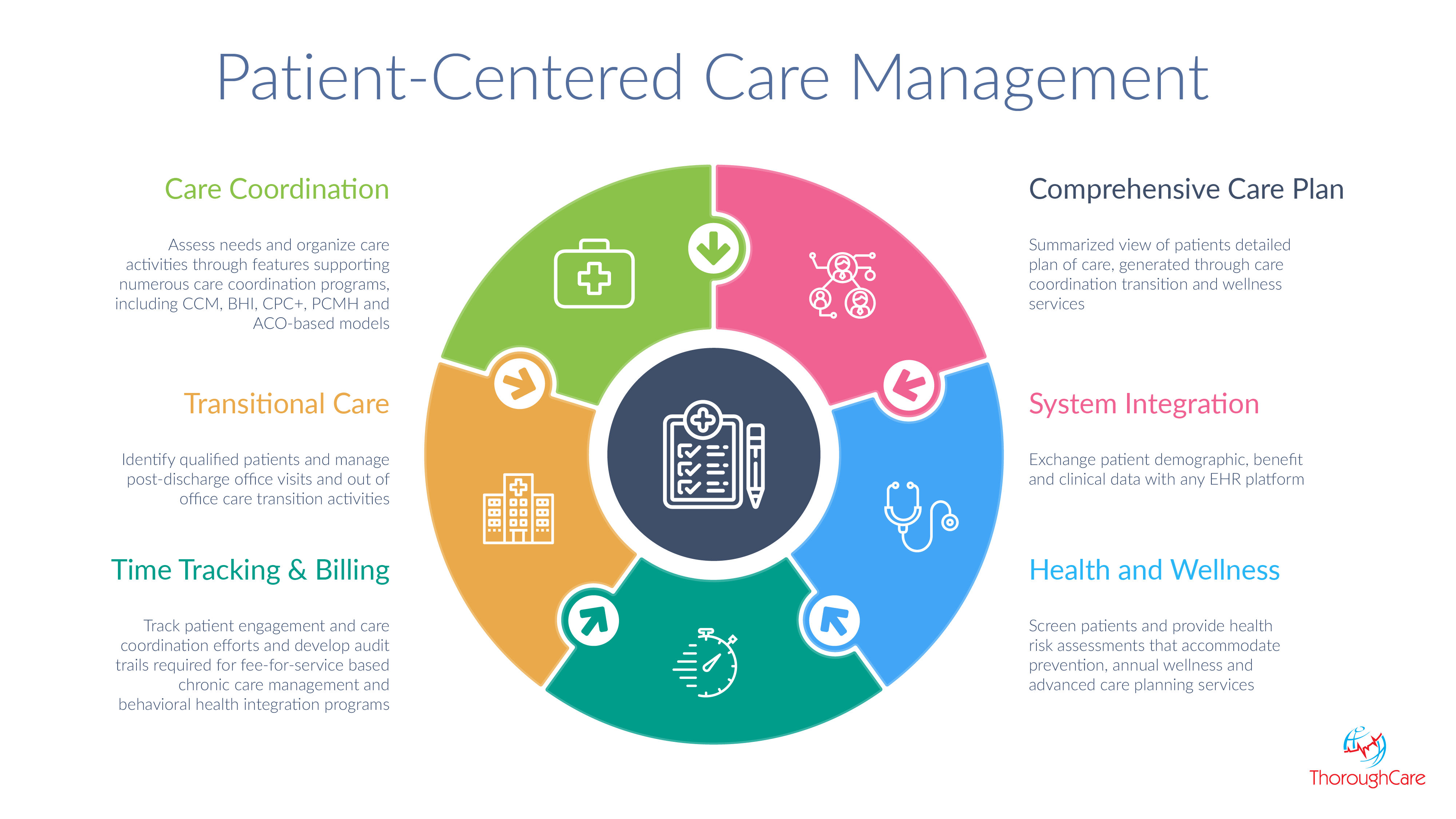
Patient-centered problem solving (PCPS) aims to empower patients in their healthcare decisions, fostering collaboration between patients and providers. However, numerous obstacles hinder its widespread adoption, while certain factors significantly enhance its effectiveness. Understanding these barriers and facilitators is crucial for improving healthcare delivery and patient outcomes.
Common Barriers to Implementing Patient-Centered Problem Solving
Several systemic and individual factors impede the implementation of PCPS. These barriers often intertwine, creating complex challenges. Time constraints, for example, frequently prevent healthcare providers from engaging in the extended discussions necessary for genuine patient partnership. Additionally, a hierarchical healthcare culture, where providers traditionally hold more power in decision-making, can stifle patient input. Furthermore, variations in health literacy among patients, along with communication difficulties, create obstacles to effective collaboration.
Finally, the lack of appropriate reimbursement models that incentivize PCPS can discourage its adoption by healthcare providers.
The Role of Healthcare System Design in Supporting or Hindering Patient-Centered Care
The design of the healthcare system itself plays a crucial role in either supporting or hindering PCPS. Systems with long wait times, fragmented care, and inflexible appointment scheduling create significant barriers to patient involvement. Conversely, systems that incorporate features like electronic health records with patient portals, convenient appointment access, and team-based care models can facilitate patient engagement and shared decision-making.
For instance, a system with readily accessible online patient portals allowing for secure messaging with providers promotes ongoing communication and empowers patients to actively participate in their care. Conversely, a system with long wait times for specialist appointments can frustrate patients and diminish their willingness to participate in collaborative problem-solving.
Impact of Healthcare Provider Training and Education on Patient-Centered Approaches
The training and education of healthcare providers are critical in shaping their approach to patient care. Providers trained in communication skills, motivational interviewing, and shared decision-making are better equipped to engage patients effectively. Curricula that emphasize patient-centered communication, active listening, and empathy foster a collaborative environment. Conversely, traditional medical training, which often prioritizes biomedical knowledge over interpersonal skills, may inadvertently hinder the adoption of PCPS.
For example, a physician trained in a communication skills workshop may be better able to elicit a patient’s preferences and concerns regarding treatment options compared to a physician who received limited training in patient-centered communication.
Strategies for Overcoming Barriers and Facilitating Patient-Centered Problem Solving
Addressing the barriers to PCPS requires a multi-pronged approach. Implementing clear communication protocols, providing adequate time for patient interaction, and fostering a culture of shared decision-making are essential. Furthermore, investing in provider training programs that emphasize communication and interpersonal skills is crucial. Integrating technology to enhance patient access to information and communication with providers can also improve patient engagement.
Finally, implementing reimbursement models that value patient-centered care can incentivize providers to adopt PCPS. For example, implementing a system of shared medical appointments, where multiple patients with similar conditions meet with a provider, can create a collaborative environment and enhance patient engagement.
Examples of Successful Interventions that Have Improved Patient-Centered Care Delivery
Several successful interventions demonstrate the effectiveness of promoting PCPS. The use of patient-reported outcome measures (PROMs) provides valuable patient-centered data that informs treatment decisions. The implementation of shared decision-making tools, such as decision aids, empowers patients to actively participate in choosing their treatment options. Furthermore, programs that focus on improving health literacy and patient communication skills can significantly enhance patient engagement and satisfaction.
For instance, the use of patient navigators, who assist patients in navigating the healthcare system and understanding their treatment options, has shown to improve patient outcomes and satisfaction. These navigators can provide crucial support and information, fostering a more patient-centered approach.
Measuring the Effectiveness of Patient-Centered Problem Solving
Evaluating the success of patient-centered problem solving (PCPS) requires a multifaceted approach, going beyond simple satisfaction surveys. Effective measurement needs to capture both the patient’s experience and the impact on their health outcomes. This involves a combination of quantitative and qualitative data, allowing for a comprehensive understanding of the effectiveness of the implemented strategies.
Methods for Evaluating the Effectiveness of Patient-Centered Problem Solving
Several methods exist for evaluating the effectiveness of PCPS. These methods range from standardized questionnaires to in-depth qualitative interviews, each offering unique insights into different aspects of the patient experience and healthcare delivery. The choice of method often depends on the specific goals of the evaluation and the resources available. For example, a large-scale study might utilize quantitative surveys to gather broad data, while a smaller, more focused study might employ qualitative interviews to gain deeper understanding of individual experiences.
Measuring Patient Satisfaction and Quality of Life
Patient satisfaction is a crucial indicator of the effectiveness of PCPS. It’s often measured using validated questionnaires like the Patient Satisfaction Questionnaire (PSQ) or the Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys. These tools assess various aspects of the patient experience, including communication with healthcare providers, access to care, and overall satisfaction with the services received. Quality of life (QoL) assessments, using instruments like the SF-36 Health Survey or the EQ-5D, measure the impact of PCPS on patients’ physical, mental, and social well-being.
Higher scores on these questionnaires generally indicate improved satisfaction and quality of life.
Using Quantitative and Qualitative Data to Assess Outcomes
Quantitative data, such as the numerical scores from satisfaction surveys or changes in clinical biomarkers, provide objective measures of PCPS effectiveness. For example, tracking the number of hospital readmissions or emergency room visits after implementing a PCPS intervention can show its impact on patient outcomes. Qualitative data, such as interview transcripts or focus group discussions, offer rich insights into the patient experience and the factors that contribute to success or failure.
For instance, interviews might reveal unmet needs or barriers to effective communication that quantitative data alone wouldn’t capture. The combination of both types of data provides a more complete picture.
Key Performance Indicators (KPIs) for Tracking Progress
Several KPIs can track progress in implementing and improving PCPS. These include: patient satisfaction scores (from surveys), reduction in hospital readmissions, improvement in quality of life scores, increase in patient activation (measured by validated scales), reduction in medication errors, and improved adherence to treatment plans. These KPIs should be chosen based on the specific goals and context of the PCPS intervention.
For instance, a PCPS initiative focused on chronic disease management might prioritize KPIs related to medication adherence and quality of life, while an initiative focused on end-of-life care might prioritize patient satisfaction and symptom control.
Summary of Methods for Measuring the Effectiveness of Patient-Centered Problem Solving
| Method | Data Type | Focus | Example |
|---|---|---|---|
| Patient Satisfaction Surveys | Quantitative | Overall satisfaction, communication, access to care | CAHPS, PSQ |
| Quality of Life Assessments | Quantitative | Physical, mental, and social well-being | SF-36, EQ-5D |
| Clinical Outcome Measures | Quantitative | Hospital readmissions, mortality rates, symptom control | Number of readmissions within 30 days |
| Qualitative Interviews/Focus Groups | Qualitative | Patient experiences, barriers, facilitators | Semi-structured interviews exploring patient perspectives on care |
Ultimately, Patient-Centered Problem Solving: Case Studies in Healthcare Delivery reveals that shifting the focus to the patient isn’t just a feel-good approach; it’s a powerful strategy to improve care quality, boost patient satisfaction, and ultimately, achieve better health outcomes. By examining real-world examples and addressing the practical challenges, we hope to inspire a future where every patient’s voice is heard and valued throughout their healthcare journey.
It’s time to rethink healthcare – one patient at a time.
Frequently Asked Questions
What are some common misconceptions about patient-centered care?
A common misconception is that patient-centered care means the doctor always does what the patient wants. It’s about shared decision-making – a collaboration where the patient’s preferences are considered alongside medical expertise to create the best treatment plan.
How can I advocate for more patient-centered care in my own healthcare?
Ask questions! Don’t be afraid to voice your concerns, preferences, and goals. Bring a family member or friend for support. Research your condition and treatment options beforehand. The more active you are in your care, the more patient-centered it will be.
Is patient-centered care more expensive?
While initial implementation costs might be higher due to increased communication and coordination, studies suggest that patient-centered approaches can lead to long-term cost savings by reducing hospital readmissions, improving adherence to treatment plans, and enhancing overall health outcomes.
